Liver Disease
The liver is a vital organ that carries out over 500 functions. Our largest internal organ, the liver has critical roles in breaking down food and storing energy, eliminating toxins, and fighting infections. Liver disorders kill over 2 million people per year, representing a significant global health challenge.
The only available therapeutic option for people with severe and end-stage liver failure is liver transplantation. Unfortunately, only about 10% of patients who need a liver transplant will receive one, and many people die waiting for a compatible donor. Stem cell research may provide alternative and novel therapies to those who do not have access to a liver transplant.
What is liver disease?
Liver diseases can have multiple causes and symptoms. Liver diseases can be inherited (have genetic causes) or can be caused by external factors. While there are multiple types of liver disease, liver damage often progresses in similar ways.
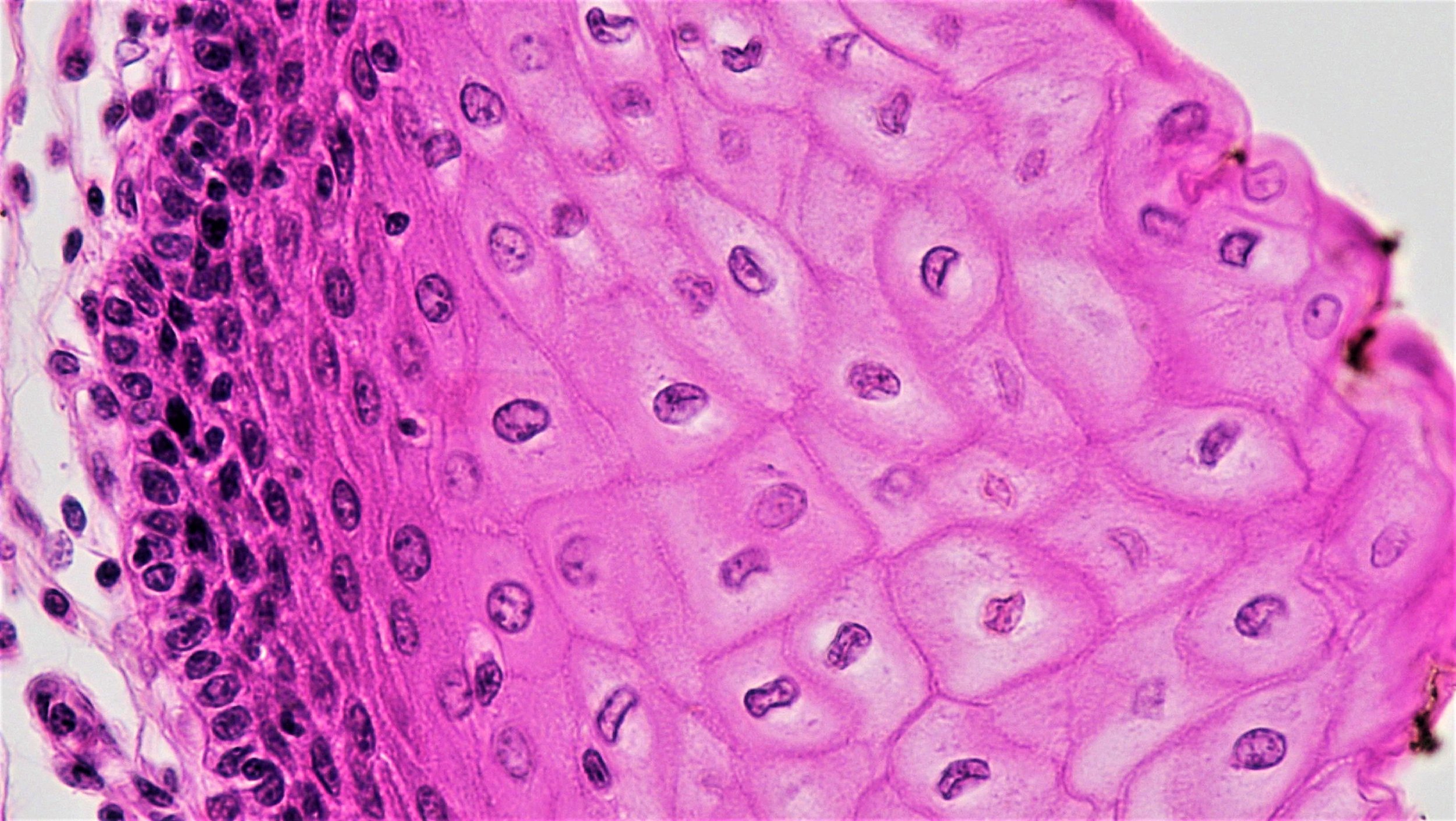
In the early stages of liver disease, the organ will become inflamed as the body tries to heal the infection or injury. At this stage of disease, the liver can regenerate if diagnosed and properly treated. If liver disease goes untreated the inflamed liver will begin to form scar tissue, which will replace healthy liver tissue. This is known as fibrosis. The buildup of scar tissue (or fibrous tissue) reduces blood flow and hinders liver function. Fibrotic livers can still heal over time.
Acute liver disease is characterized by widespread death of liver cells and rapid deterioration of liver function. More common is chronic liver disease, when multiple factors such as obesity, alcohol, viral infections, or immune diseases, can cause chronic scarring of the liver. Both acute and chronic liver disease can be life-threatening.
Chronic scarring of the liver, or cirrhosis, caused by long term damage, can be a serious life-threatening condition that can lead to liver cancer or liver failure. Once a liver has reached liver failure it has lost all or almost all of its function and the patient needs immediate medical attention. Treatment options are limited at this stage.
Liver Regeneration
The liver is our only internal organ that can regenerate after damage. This regeneration is partially due to the major cell type in the liver, the hepatocyte. Hepatocytes are critical for synthesizing proteins and lipids, metabolizing carbohydrates, and detoxifying functions of the liver. Hepatocytes can normally divide to replace cells that die and they can even repair some damage to the liver. Another cell type known as hepatic biliary cells, which drain bile, can also orchestrate liver repair. Liver disease that causes damage to hepatocytes or biliary cells reduces the liver’s ability to recover. In cases of severe injury, specialized cells known as hepatic progenitor cells are thought to take over regeneration. The formation of scar tissue can limit the ability of the liver to repair itself. Studies are ongoing to determine whether there are stem cells in the adult liver, and if there are, how they function and replenish the liver.
Causes of Liver Disease:
Liver disease can have genetic causes or be caused by external factors, such as viruses, alcohol, and obesity.
Genetics: Inherited liver diseases include hemochromatosis, Wilson's disease, Alpha-1 antitrypsin deficiency, tyrosinemia, and Crigler–Najjar syndrome. These inherited metabolic disorders can cause excessive buildup of certain substances in your liver and predominantly affect the hepatocyte.
Infection: The liver can be infected by parasites or viruses, most commonly hepatitis, which lead to inflammation that impairs the liver. Viruses can be spread through contaminated food or water, contact with an infected individual, or through blood or semen.
Autoimmune diseases: In certain autoimmune diseases, such as autoimmune hepatitis, primary biliary cholangitis, and primary sclerosing cholangitis, the immune system attacks the liver, leading to liver disease.
Cancer: Multiple types of cancer can affect the liver, including liver cancer, bile duct cancer, and liver adenoma. Liver cirrhosis, chronic hepatitis infection, diabetes, nonalcoholic fatty liver disease, exposure to certain toxins, and excessive alcohol use can increase chances of liver cancer.
Other causes: Liver disease is also commonly caused by long term alcohol abuse, accumulation of fat in the liver, and by certain prescription or herbal medications. Additional risk factors including diabetes, family history of liver disease, tattoos or piercings, and sharing needles.
How is liver disease currently treated?
Whether or not liver disease can currently be treated depends on the specifics of the disease state and cause(s). Changes to lifestyle, such as reductions in alcohol consumption or weight loss, can improve some liver function depending on the underlying problem. Some liver diseases can be treated with medicine or surgery, while certain metabolic liver diseases can be treated by reducing specific substances in the body, such as iron or copper.
Liver disease that has progressed to severe or end stage chronic liver disease, however, may ultimately require a liver transplant. In a liver transplant the diseased liver is removed and replaced with the healthy liver from a deceased donor or with part of a liver from a healthy living donor.
A liver transplant has multiple risks including rejection of the organ, negative side effects of immunosuppression, infection, bleeding, clotting, and failure of the donated liver. It is also possible that the liver disease reoccurs in the transplanted liver.
Unfortunately, the number of patients waiting for a liver transplant far exceeds the number of available donors. Many people may die while waiting for a liver transplant. New treatments are needed to help the millions of people living with liver disease worldwide.
How are we using stem cells to understand and treat liver disease?
Scientists are using stem cells to better understand liver disease, to identify potential new drugs to treat liver disease, and as a potential source of replacement cells. Several types of liver disease may potentially be treated by stem cell-based therapies including metabolic liver diseases, acute liver failure, and chronic liver disease.
Researchers are using pluripotent stem cells in the laboratory to study liver disease and its treatments. Cells from skin or blood can be “induced” to become cells that are in an embryonic-like state, known as induced pluripotent stem cells. These cells can then be coaxed to become any cell type in the body. Scientists have figured out how to mimic various stages of embryonic development to obtain stem cell-derived hepatocytes from induced pluripotent stem cells. These stem cell-derived cells have been shown to metabolize food, store energy, and eliminate toxins similarly to normal liver cells. These induced pluripotent stem cells can grow indefinitely in the lab and can potentially be used to generate large numbers of hepatocytes that could have clinical use.
Scientists are studying stem cells to:
Understand normal liver disease and regeneration: The liver is the only internal organ capable of regeneration. Regeneration in the normal liver is thought to be carried out by specialized cells, including hepatocytes and hepatic progenitor cells. By studying normal liver development and regeneration, scientists might uncover new ways to treat patients with liver disease.
Improve diagnostic tools and identify new drugs: Induced pluripotent stem cells can be derived from patients with a variety of types of inherited liver disease. These stem cells can then be used to produce hepatocytes with the same genetic abnormality as the patient. Scientists can study how these hepatocytes differ from normal hepatocytes and also use them to identify new medications that could help with treatment. Studying stem cell models of liver disease can allow scientists to further understand what happens during progressive inflammation and scarring to better target future treatments. It is critical to diagnose liver disease as early as possible to give patients the best chance for treatment and repair. Studying various patient-derived hepatocytes could also uncover ways to understand liver disease and its progression, hopefully leading to advances in diagnosing liver disease more quickly.
Develop cell-based approaches to treat liver disease:
Scientists are hoping to one day transplant stem cell-derived hepatocytes into patients so that these new hepatocytes can take over normal functions of the liver. There are currently several obstacles to this approach. Transplanted cells need to be able to properly attach to and integrate into the patient’s liver and current attachment rates can be quite low. Additionally, preexisting scar tissue can impact the function of the newly transplanted cells. Transplanted cells are at risk for being rejected by the patient’s immune system (transplant rejection) and it is currently difficult to produce hepatocytes in sufficient numbers for transplantation. Induced pluripotent stem cell-derived hepatocytes can help address these last two issues. If induced pluripotent stem cells are derived from the patient, the hepatocytes they generate will be genetically identical to the patient and will not be rejected and scientists are working on methods to scale up the production of these cells. Research is ongoing to improve cell therapies that might help a variety of liver diseases including:
Inherited metabolic liver disease: The genetic cause of certain inherited metabolic liver diseases has been identified. In these cases, iPSC-derived hepatocytes could be genetically corrected, using a process such as CRISPR. Replacing diseased hepatocytes with gene corrected functional hepatocytes may be sufficient to have clinical benefit. Examples of diseases where this may be possible include Tyrosinemia type 1 and Crigler–Najjar syndrome type I (which causes hyperbilirubinaemia).
Acute liver failure: While acute liver failure might be complicated by the development of multiorgan failure, which would require distinct management, the replacement of healthy hepatocytes may also be sufficient to treat this disease effectively.
Chronic liver disease: For chronic liver disease, and its end-stage manifestation of cirrhosis, the situation is more complex as the simple replacement of hepatocytes may not be adequate to correct disease. This is because the degree of scarring and inflammation may prevent the transplanted cells from surviving and integrating effectively. For liver cirrhosis it may therefore be necessary to develop therapies that target the scarring and inflammation as well as replacing or supplementing the damaged hepatocytes or biliary cells. These studies are ongoing.
Bio-artificial livers: Researchers are also using stem cell-derived hepatocytes to engineer external devices that would function like an artificial liver similar to kidney dialysis machines. In this alternative to transplantation, living hepatocytes would be used to make a bio-artificial liver, which could be used to treat liver disease by performing normal liver functions externally, such as clearing toxins and producing critical proteins. Such a device could also help extend the time before a patient needs a transplant.
What is the clinical status of cell-based therapies for liver disease?
There have been several cell-based clinical studies for liver disease of various types, including acute and metabolic liver disease as well as liver cirrhosis.
Inherited metabolic liver disease: There have been encouraging clinical results from hepatocyte transplantation for a variety of metabolic liver diseases such as Crigler-Najjar syndrome, glycogen storage disease type 1, and urea cycle disorders. Continued research is necessary to optimize methods for efficiently producing sufficient numbers of hepatocytes.
Chronic liver disease: Currently there is no clear evidence that cell therapy is effective for treating liver cirrhosis. There have been a number of small studies that have shown some possible benefit, but larger randomized controlled clinical trials have so far failed to show positive outcomes. As such, treating cirrhosis with cell therapies cannot be recommended outside of properly controlled clinical trials.
Considerations for cell-based therapies and clinical trials
While there are ongoing clinical trials, more testing is needed to know whether these cell-based treatments for liver disease will be safe and effective. Visit Clinical Trials or Stem Cell Treatments if you are considering participating in a clinical trial or a stem cell “treatment”. You should always be sure consult a trusted medical professional before deciding to proceed with a treatment or trial.
Useful Links
March 2019