Diabetes
Nearly 400 million people worldwide are living with diabetes, and that number is expected to jump to almost 600 million by 2035, according to the International Diabetes Federation. For many people, diabetes can be controlled with diet, exercise and, often, insulin or other drugs. However, complications from diabetes can be serious and include kidney failure, nerve damage, vision loss, heart disease and a host of other health issues.
What is diabetes?
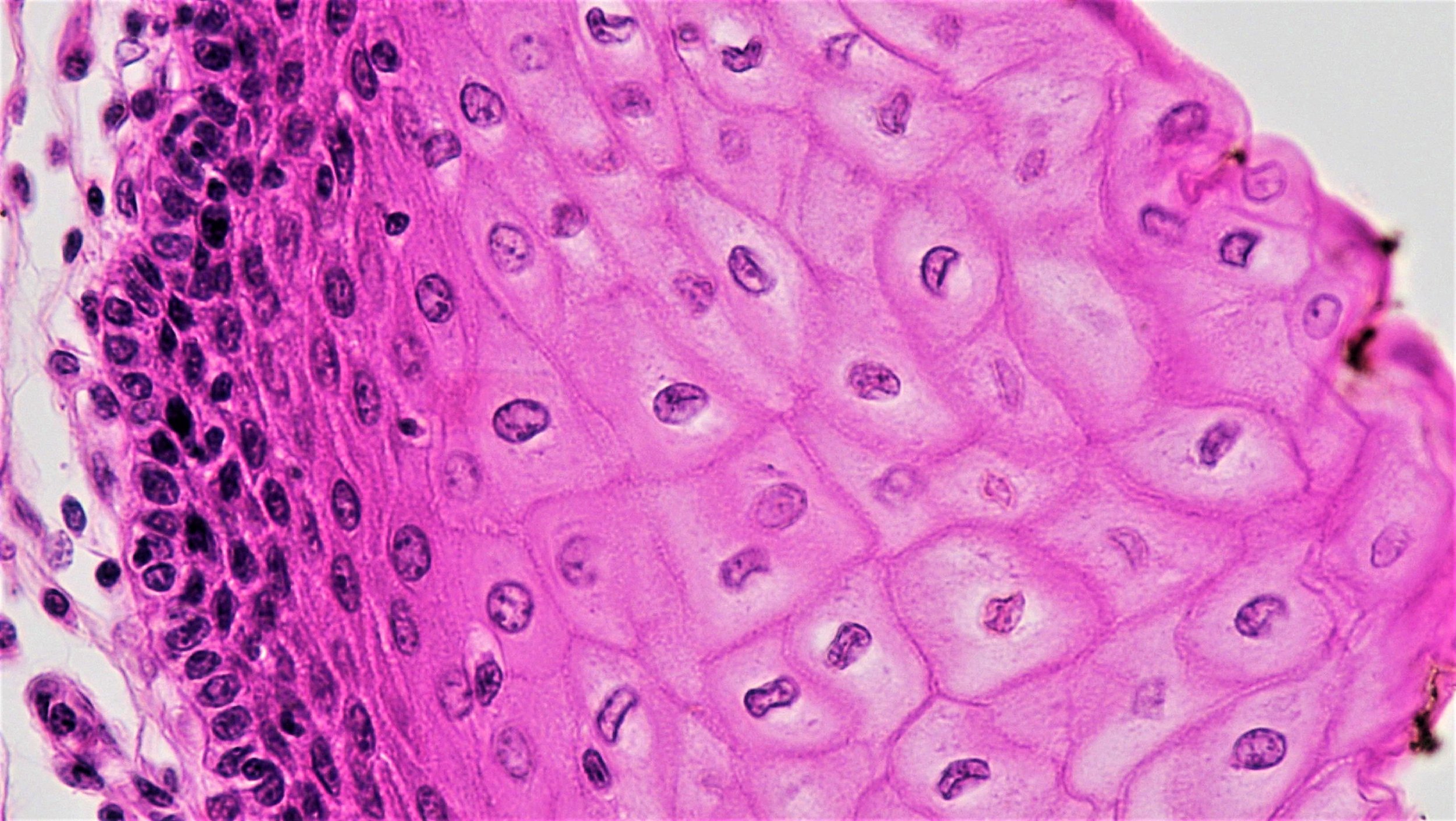
At its most basic, diabetes is a condition in which the body cannot regulate or properly use sugar (called glucose) in the blood. The pancreas plays a critical role in controlling these levels. Within the pancreas are hundreds of thousands of cell clusters, known as the islets of Langerhans, which contain multiple types of hormone-producing cells that regulate blood glucose. Most importantly, these include beta cells, which produce a hormone known as insulin that is released into the bloodstream when blood sugar levels reach a certain threshold, signaling other cells in the body to take up sugar, a major energy source for the body’s cells.
The human body is constantly balancing the amount of available blood sugar -- levels that are either too high or too low can be harmful. In diabetes, blood sugar is elevated either because the pancreas does not produce enough insulin (type 1 diabetes) or because or cells in the body fail to respond to the insulin that is released (type 2 diabetes).
Type 1, previously known as juvenile diabetes. In type 1 diabetes, the body’s immune system attacks the beta cells in the pancreas. When the beta cells are lost there is not sufficient insulin for proper control of glucose levels. Resulting high sugar levels in the blood can cause damage to the kidneys, eyes, nervous system, and other organs. People of all body types can be diagnosed with type 1 diabetes at any age.
Type 2 diabetes, previously known as adult-onset diabetes. In type 2 diabetes, cells in the body become resistant to insulin. They don’t respond well to the insulin released by beta cells. The beta cells produce more insulin to signal the other cells, but eventually are not able to compensate. As with type 1, high blood sugar levels in type 2 diabetes can cause serious damage to the body. The incidence of type 2 diabetes increases in people over 45 but type 2 is increasingly diagnosed in younger individuals. Genetic background, obesity, and lack of exercise are common risk factors that predispose to type 2 diabetes.
How is diabetes treated?
Type 1 diabetes patients are given insulin to help them control their glucose levels. These patients, however, often struggle to optimally balance their blood sugar and they need to monitor their blood sugar multiple times a day. New technologies, such as multiple types of insulin pumps, have greatly improved treatment for some people, enabling the delivery of individualized doses or a steady stream of insulin, but they cannot precisely mimic the healthy human body’s constant, sophisticated monitoring and adjusting of insulin production provided by normal beta cells.
Type 2 diabetes can sometimes be controlled with diet and exercise. However, many people with type 2 diabetes eventually have to take insulin injections to control blood sugar levels and/or other medications to deal with complications from the disease.
There have been great advances in reducing the toll from diabetes-related complications through improvements in insulin administration and glucose monitoring, but the ideal treatment will be the replacement of the missing insulin-producing pancreatic beta cells. Since 1999, several hundred people with type 1 diabetes have received islet transplants. Many of these people have been able to stop taking insulin for at least a few months or years. However, most patients have to begin taking insulin again within four years after the procedure. Relatively few transplants are done because of the short supply of islets, the need for immunosuppression, and the expense.
Transplants generally are less effective in type 2 diabetes patients because they require more islets due to their resistance to insulin.
How are we using stem cells to understand diabetes?
Stem cells are being used for ongoing research to help us explore the intricate ways in which our bodies process sugar and answer some important questions about the root causes of diabetes, such as:
In type 1 diabetes, why does the immune system begin to attack beta cells and not other cells in the pancreas or in other organs or tissues?
In type 2 diabetes, what causes the resistance to insulin?
Recently, there has been great progress in generating beta cells from embryonic stem cells and induced pluripotent stem cells. Laboratory studies help us better understand disease progression, what the potential genetic causes may be, and similarities and differences between patients. Researchers are using this information to try to diagnose people earlier, prevent disease progression, and more effectively treat diabetes.
Induced pluripotent stem cell-derived beta cells could also be used for beta cell replacement therapy, providing what could potentially be a cure if they can be successfully transplanted into patients. As induced pluripotent stem cells could be made from the individual patient, the resulting beta cells would avoid transplant rejection, but recipients with type 1 diabetes would still face autoimmune attacks on their beta cells.
What is the potential for stem cells to treat diabetes?
Developing and testing a truly effective stem-cell based treatment for diabetes will take years. The two main challenges are finding an adequate supply of insulin-producing cells and protecting these cells from attack by the immune system. There has been impressive progress in solving the beta cell supply problem in that it is now possible to generate insulin-producing cells from human embryonic stem cells and induced pluripotent stem cells.
Researchers are looking at ways to restore the number of functional beta cells in patients with diabetes, pursuing both the replacement of lost beta cells and the protection of beta cells from further damage. Several different approaches are being used, including:
Making beta cells from embryonic stem cells or induced pluripotent stem cells. Embryonic stem cells and induced pluripotent stem cells can be grown in large number in the laboratory and have the potential to be coaxed into becoming any cell type in the body, including glucose sensing, insulin-producing beta cells. Recent leaps forward in these technologies make this a very promising avenue for generating large numbers of replacement beta cells.
Stimulating beta cells to make many more copies of themselves. Beta cells can do this in the pancreas, but usually very slowly, and less and less as we get older. Researchers are looking for drugs that might enhance this self-renewal as a possible treatment for people with type 2 or early-stage type 1 diabetes.
Protecting beta cells from immune attack. Immunologists and bioengineers are working on a range of strategies to protect transplanted cells from immune attack. One approach is to use cellular engineering to make the cells more resistant to such an attack and another is to encapsulate the cells within semi-permeable membranes to protect them from the cells of the immune system. Such capsules are porous and would allow small molecules such as glucose and insulin to pass through while protecting the beta cells from the cells of the immune system.
Key to these approaches is getting beta cells into a place in the body where they can work and protecting them from what was damaging them in the first place. This includes transplantation into parts of the body where the replacement cells are less likely to be attacked by the immune system or placement of the cells into protective capsules. Such capsules are porous and would allow small molecules such as glucose and insulin to pass through while protecting the beta cells from the cells of the immune system.
For type 1 diabetes, there are a number of experimental approaches being taken to curb the immune system’s attack on the beta cells. Most of these are still being explored in the lab. There are some clinical trials underway to test whether blood stem cells or mesenchymal stem cells from the bone marrow might alter or re-set the immune system so that it no longer attacks the beta cells. However, the mechanisms underlying how this use of these cells would work are not well understood, and further research is needed to establish whether any of these approaches will prove safe and effective.
What is the clinical status of cell-based therapies for diabetes?
There are a number of experimental approaches being taken to curb the immune system’s attack on the beta cells. New cell-based therapies being developed must be tested in rigorous clinical trials that comply with regulatory standards, such as those recommended by the US Food and Drug Administration. Some clinical trials which have been approved by regulators are underway in which insulin-producing cells derived from ESCs are being placed into encapsulation devices and transplanted into patients with type 1 diabetes, but clinical benefit has not yet been reported. There have been a variety of claims in recent years of beneficial results from unregulated transplants using a patient’s own adult stem cells, but these approaches are not supported by a current understanding of science and lack independent and objective efficacy data. These treatments and the clinics offering them should be avoided.
There continue to be high hopes and expectations that cells derived from stem cells will succeed for beta cell replacement therapy and thus essentially cure type 1 diabetes. We know that insulin-producing cells derived from embryonic stem cells and induced pluripotent stem cells can reverse diabetes in experimental animals. A great deal of work on this problem is going on in companies and academic research centers. The calendar for successful clinical application is uncertain but progress toward this goal continues to be exciting.
Useful Links
March 2019