Heart Disease
Cardiovascular disease is the number one cause of death worldwide in men and women worldwide, claiming more than 17 million lives each year. The effects of acute myocardial infarction (heart attack) and congestive heart failure present great challenges for doctors and researchers alike. Heart attacks cause damage to the heart muscle, making it less efficient at pumping blood throughout the circulatory system. The heart has minimal ability to regenerate, so the lost muscle is replaced by scar tissue. This leaves patients with reduced cardiac function, which often progresses to heart failure, where the heart cannot meet the body’s demand for blood flow. Current treatments for heart failure focus on managing symptoms (like reducing blood pressure) but do not address the root problem: a heart that has lost too many functional heart muscle cells. Despite major advances in how heart disease is managed, heart disease is progressive. Once heart cells are damaged, they cannot be replaced by the body. New treatment strategies are needed to restore function, rather than manage, this chronic disease.
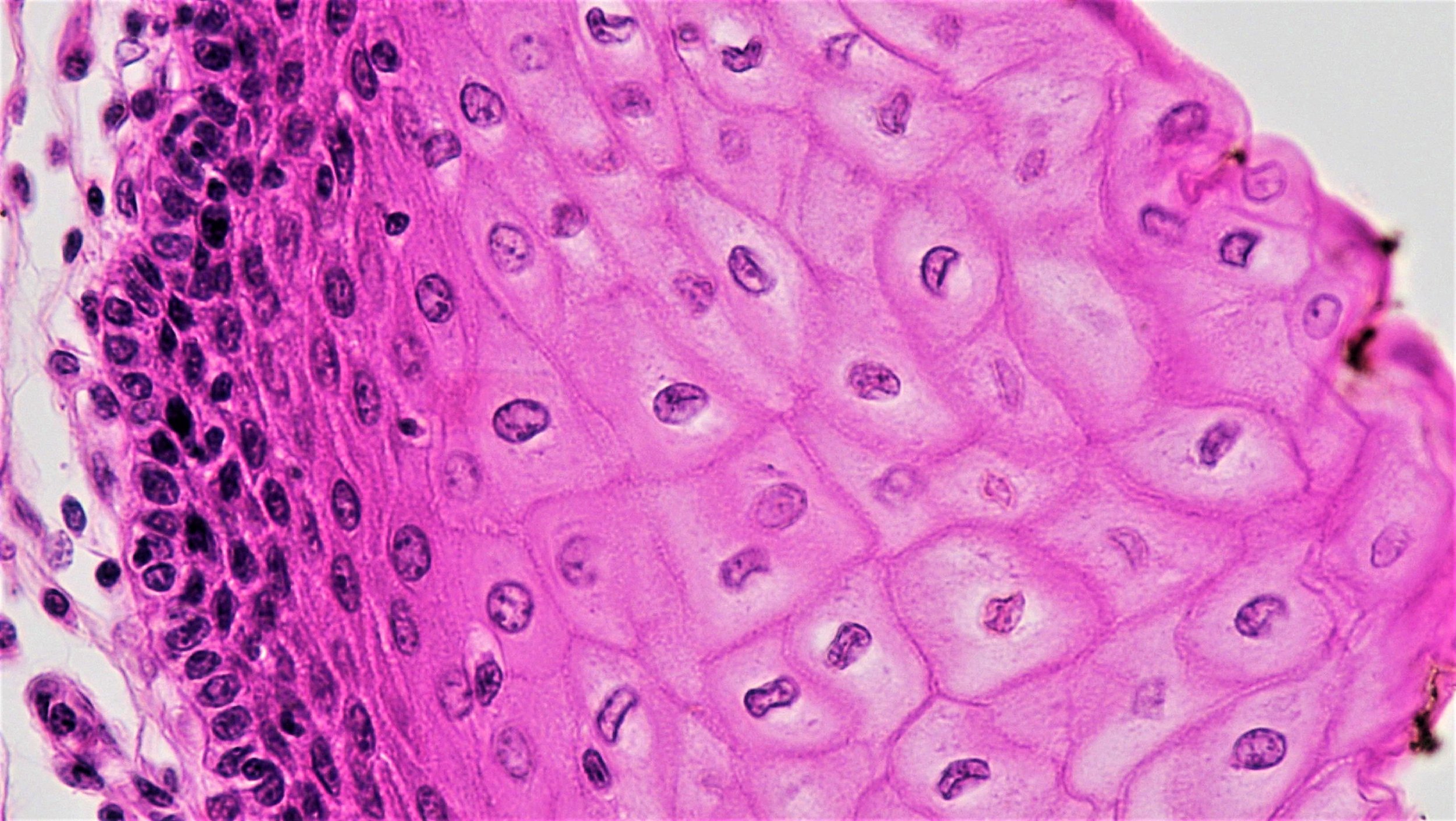
Close up of a mouse heart stained to reveal the important structural protein that helps heart muscle cells to contract (red). The cell nuclei are labeled in magenta. | Gladstone Institutes
What is acute myocardial infarction?
Acute myocardial infarction, or a heart attack, occurs when the blood vessels that feed the heart are blocked, often by a blood clot that forms on top of a plaque, a build-up composed of fat, cholesterol, calcium, and other elements found in the blood. Without oxygen and other nutrients from the blood, heart cells die and large swaths of heart tissue are damaged.
After a heart attack, scar tissue often replaces the damaged part of the heart muscle, and this scar tissue impairs the heart’s ability to keep beating normally and pumping blood efficiently. The heart ends up working harder, which weakens the remaining healthy sections of the heart and over time, the patient experiences more heart-related health issues.
What is congestive heart failure?
Heart failure is a condition in which the heart’s blood-pumping action is weaker than normal. Blood circulates more slowly, pressure in the heart increases, and as a result, the heart is unable to pump enough oxygen and other nutrients throughout the body. To compensate, the chambers of the heart may stretch to hold more blood, or the walls of the chambers may thicken and become stiff. Eventually, the kidneys respond to the weaker blood-pumping action by retaining more water and salt, and fluid can build up in the arms, legs, ankles, feet, and even around the lungs. This general clinical picture is called congestive heart failure.
Many conditions can lead to congestive heart failure. Among the most common are heart attacks, high blood pressure, valve disease, and genetic conditions called cardiomyopathies.
How are acute myocardial infarction and congestive heart failure currently treated?
Heart cells beating in a culture dish | Gordon Keller Lab
Lifestyle changes, such as lowering salt and fat intake, exercising regularly, reducing alcohol consumption, and quitting smoking are recommended to reduce the chances of heart attack and in the early stages of congestive heart failure. The goals are to slow down any progression of the disease, lessen symptoms, and improve quality of life.
To treat acute myocardial infarction, doctors often use a procedure called angioplasty to disrupt the blood clot and widen clogged arteries. Angioplasty involves inserting and inflating a tiny balloon into the affected artery. Angioplasty may be combined with the insertion of a small wire mesh tube called a stent, which helps keep the artery open and reduces the chances that it will get blocked again.
Other post-heart attack treatments include the regular use of blood thinners (for example, low-dose aspirin) to prevent new clots from forming and other medications to help control blood pressure and blood cholesterol levels. Beta blockers are often prescribed after a heart attack or to treat high blood pressure and ACE inhibitors can prevent heart failure from progressing.
For moderate to severe congestive heart failure, surgery may be necessary to repair or replace heart valves or to bypass coronary arteries with grafts. In severe cases, patients may have pacemakers or defibrillators implanted to control heart rhythms. For more information on heart failure and other cardiovascular diseases visit the American Heart Association.
How are we using stem cells to understand heart function and disease?
Researchers are using stem cells in two important ways to improve cardiac health. First, they are turning stem cells into “heart muscle in a dish.” If patients have genetic causes of heart disease, their stem cell-derived heart muscle also will have this disease and this heart muscle can be used to discover new drugs. Second, stem cells offer ways to replace damaged heart tissue. Using cellular therapy, researchers hope to repair or replace heart tissue damaged by congestive heart failure and heart attacks. Unlike the treatments listed above, cellular therapy could provide a durable treatment for heart deficiencies, rather than symptom-focused treatment.
Your heart is constructed of several types of cells. For mending damaged heart tissue, researchers generally focus on three specific heart cell types:
Cardiomyocytes, the beating muscle cells that make up the atria, the chambers where blood enters the heart, and the ventricles, where blood is pumped out of your heart. Cardiomyocytes are currently being targeted in cellular therapies for heart disease.
Cardiac pacemaker cells, which send and receive electrical signals to keep your heart beating in rhythm.
Endothelial cells, which line blood vessels and help deliver oxygen to the cardiomyocytes.
Researchers are experimenting with a variety of stem cell therapies to transplant new cells, use tissue engineering to improve the survival or function of transplanted cells, and stimulate existing cells to generate new cardiomyocytes.
Researchers can grow cardiomyocytes in the lab from the following sources:
Embryonic stem cells, cells derived from embryos that can give rise to all cells in the body.
Induced pluripotent stem cells, adult tissue-specific cells that are reprogrammed in the lab to behave like embryonic stem cells and which have the capacity to become any cell type in the body, including cardiomyocytes.
Strikingly, these stem cell-derived cardiomyocytes will beat in unison in a culture dish, the same way they do in a living heart muscle. This property is essential, as researchers explore whether they might someday grow replacement tissue for transplantation into patients. However, it is not yet known whether lab-grown cardiomyocytes will integrate or beat in unison with surrounding cells if they are transplanted into a beating human heart.
Cardiac cells made from induced pluripotent stem cells are also incredibly useful for creating human models of heart disease to better understand exactly what goes wrong and for testing different drugs or other treatments. They can also be used to help predict which patients might have toxic cardiac side effects from drugs for other diseases such as cancer.
What is the clinical status of cell-based therapies for heart disease?
Since heart failure after heart attacks results from death of heart muscle cells, researchers have been developing strategies to “remuscularize” the damaged heart wall in efforts to improve its function. Researchers are transplanting different types of stem cell and progenitor cells (see above) into patients to repair the damaged heart muscle. These strategies have mainly used either “adult” stem cells (found in bone marrow, fat, or the heart itself) or “pluripotent” stem cells.
Preliminary results from experiments with adult stem cells showed that they appeared to improve cardiac function even though they died shortly after transplantation. This led to the idea that these cells can release signals that can improve function without replacing the lost muscle. Clinical trials began in the early 2000s transplanting adult stem cells from the bone marrow and then from the heart. These trials demonstrated that transplanting cells into damaged hearts is feasible and generally safe for patients. However, larger trials that were randomized, blinded, and placebo-controlled, showed fewer indications of improved function. The consensus now is that adult stem cells have modest, if any, benefit to cardiac function.
Research shows that pluripotent stem cell-derived cardiomyocytes can form beating human heart muscle cells that both release the necessary signals and replace muscle lost to heart attack. Transplantation of pluripotent stem cell-derived cardiac cells have demonstrated substantial benefits to cardiac function in animal models of heart disease, from mice to monkeys. Recently, pluripotent stem cell-derived interventions were used in clinical trials for the first time. “Patches” of human heart muscle cells derived from the stem cells were transplanted onto the surface of failing hearts. Early results suggest that this approach is feasible and safe, but it is too early to know whether there are functional benefits.
Research is ongoing to test cellular therapies to treat heart attacks by combining different types of stem cells, repeating transplantations, or improving stem cell patches. Clinical trials using these improved methods are currently targeted to begin around 2020.
Unfortunately, many unscrupulous clinics are making unsubstantiated claims about the efficacy of stem cell “therapies” for heart failure, creating confusion about the current state of cellular approaches for heart failure. To learn more about warning signs of these unproven interventions, please visit “Nine Things to Know About Stem Cell Treatments.”
Useful Links
October 2018