Human Fetal Tissue Research
Since the 1930s, human fetal tissue (HFT) and cells derived from it have been crucial in advancing science and medicine due to their unique features and capabilities, such as the ability to divide and create more cells efficiently, adaptability to lab environments, and increased potential to develop into different cell types. Many people have benefitted, and millions of lives have been saved thanks to HFT research. This work allows scientists to study normal development, developmental disorders, infectious diseases, and more, enhancing our overall understanding of human biology.
While the specific uses for HFT are extensive, we have highlighted three key research areas that demonstrate the high value of HFT research for public health.
Vaccine Development and Production
Every year, vaccines save millions of lives globally. Scientists have used HFT for developing vaccines, including those that protect against polio, chickenpox, shingles, measles, rubella, rabies, hepatitis A, and COVID-19. Cells derived from HFT are commonly used in the early stages of vaccine development as they can expand in culture and produce large amounts of the target virus that will eventually be used to create a reliable and consistent vaccine. It is important to note that while fetal cell lines are still used to generate vaccines, no fetal cells are included in the final immunization.
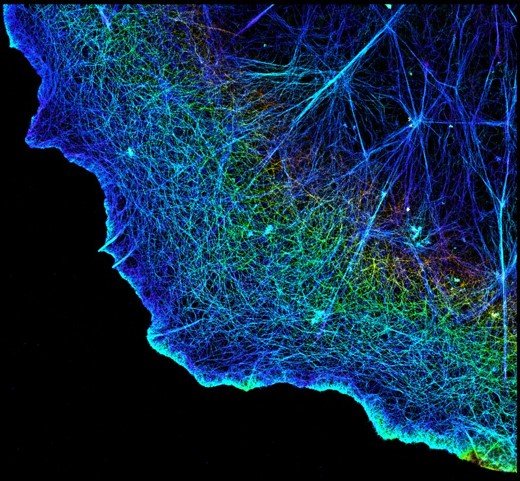
Studying Development and Disease
To understand the origins of disease and develop effective treatments, scientists must research the developmental process in both normal and abnormal tissue. While animal models are useful to understand the complex biology of a living system, there are many differences that exist between human and animal systems that influence the way cells and tissue function. Therefore, HFT is an essential resource to study human development and disease, including research on conditions like diabetes and Alzheimer’s disease.
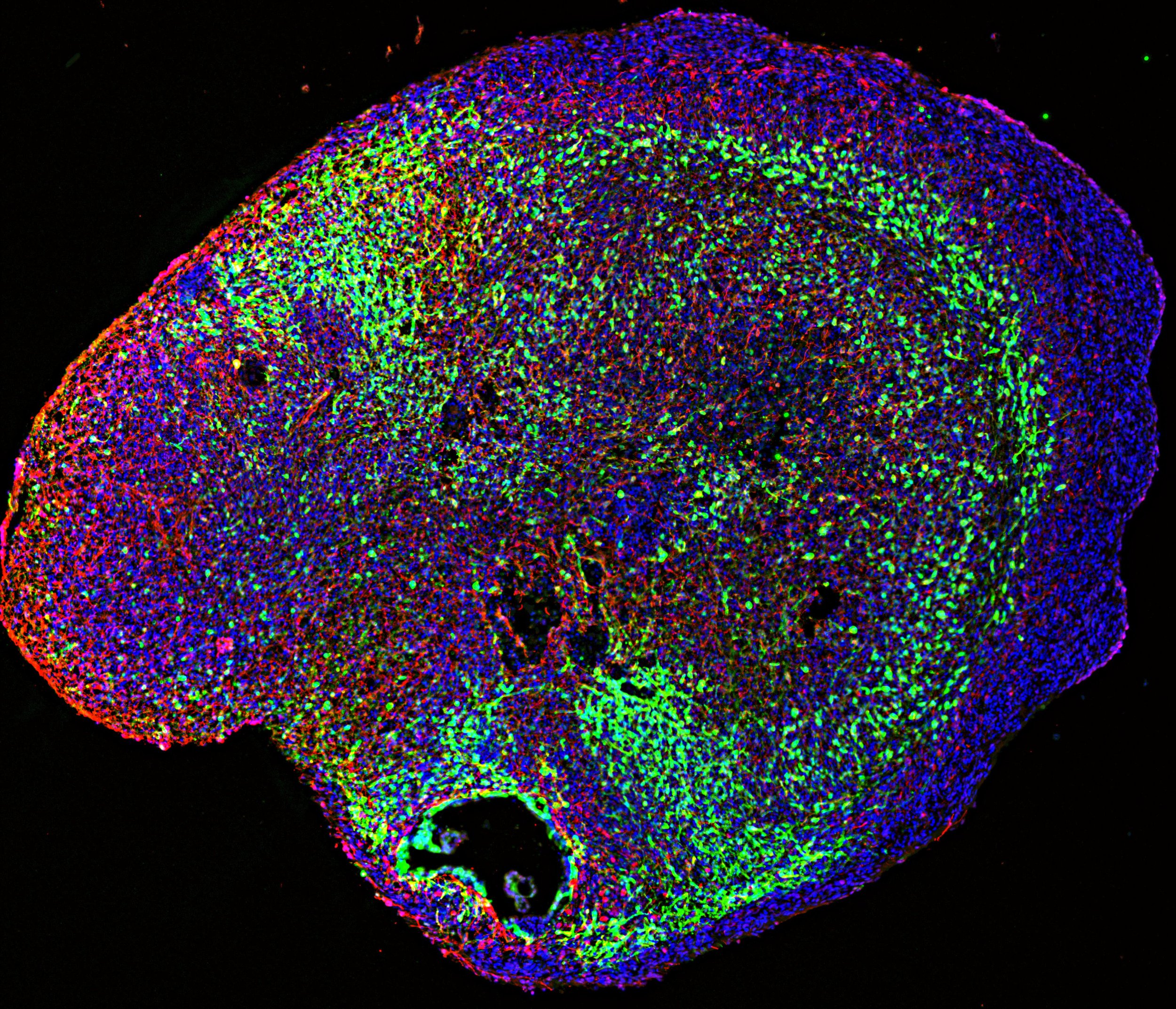
Gold Standard for Model Systems
When scientists develop cell and tissue models in the lab, they need to be validated and optimized to ensure these model systems are accurate and reliable to be used for future research and clinical applications. HFT is the gold standard for comparing these alternative model systems as a source of an authentic human developmental context. Despite the emergence of alternatives, it is crucial to recognize that animal models and alternative cell sources do not currently possess the necessary properties to fully replace HFT in scientific research. While alternatives may reduce reliance on HFT, it is not possible to fully leverage the alternatives without further validation using HFT. The ongoing need for HFT validation underlines its irreplaceable role in biomedical research and therapeutic efforts.
Collectively, research using HFT has saved millions of lives, decreased healthcare costs, deepened our understanding of human biology, and significantly improved human health. Importantly, research involving HFT is tightly regulated with appropriate and rigorous oversight. Researchers must follow all requirements to ensure ethical and responsible use of this valuable resource. Moving forward, HFT will continue to be an essential resource for driving biomedical progress and ultimately improving global public health.
Acknowledgements:
Kendra Prutton, International Society for Stem Cell Research (ISSCR)
Justin Brumbaugh, University of Colorado
Brian Aguado, University of California, San Diego
Tamra Lysaght, National University of Singapore
Lawrence Goldstein, Sanford Consortium for Regenerative Medicine
Kym Kilbourne, International Society for Stem Cell Research (ISSCR)
Jack Mosher, International Society for Stem Cell Research (ISSCR)
Tyler Lamb, International Society for Stem Cell Research (ISSCR) 2024
January 2024